Slide Show - Understanding Melanoma
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about melanoma which will help other patients, caregivers and families.










*Please note: This slide show represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
Melanoma is a type of cancer that begins most often in the skin. Less frequently, melanoma can occur in the eye or in mucous membranes such as the nasal passages, mouth, throat, vagina, or rectum.
Melanoma develops in cells called melanocytes that give our skin its color. It is the most serious form of skin cancer because it can spread to any part of the body and could become fatal. The spread of cancer is referred to as metastasis.
The skin is the body’s largest organ, with a total area of about 20 square feet. The skin performs many functions: It is a barrier that protects us from germs and the weather. It helps regulate body temperature. It allows us to sense heat, cold, touch, and pain.
Lymph nodes – small organs made up of clusters of different types of cells that belong to the immune system – are located throughout the body. Some are close to the skin, others are in deeper tissues. When melanoma starts to spread, it often travels first to a nearby lymph node and grows there.
Cancer starts when cells become malignant – that is, they start to grow and divide uncontrollably, forming a tumor, and gain the ability to spread to other parts of the body. Melanoma is caused by melanocytes that have become malignant.
Ultraviolet, or UV, rays, are a major cause of melanoma. Most UV comes from sunlight. UV rays can also come from other sources, such as tanning beds.
UV damages the genetic material, or DNA, in melanocytes and skin cells. This causes changes in the genes that control how the cells grow and divide. Over time, these cells may become malignant. The damage to DNA may occur many years before cancer develops.
Some gene changes that increase risk for melanoma run in families. These gene changes are called mutations. Around one out of every 10 people who get melanoma have at least one close relative – such as a parent, child, or sibling – who also had melanoma. A parent with a mutation has a 50-50 chance of passing it on to a child.
The most important sign of melanoma is a new spot, or mole, on the skin; a spot that is changing in size, shape, or color; a spot that bleeds; or an “ugly duckling” that looks different from other spots. Doctors call spots like these lesions. A lesion is an area of abnormal or damaged tissue.
Other signs to look for are a sore on the skin that doesn’t heal or a mole that’s red, swollen, itchy, tender, bleeding, or painful.
Look for these signs when checking moles on your skin:
A – An asymmetrical, or irregular, shape
B – An irregular or uneven border
C – More than one color in the same lesion
D – A diameter bigger than a pencil eraser (about 6 millimeters)
E – evolution, or change, in the size or color of a mole.
If you notice any of these signs, make an appointment right away to have a dermatologist or primary care physician examine your skin.
Staging is a system for describing the size of the main tumor, whether it has spread, and if so, how far.
Stage 0 melanoma is confined to the top layer of the skin. Doctors call it melanoma in situ, which means “in its original place.”
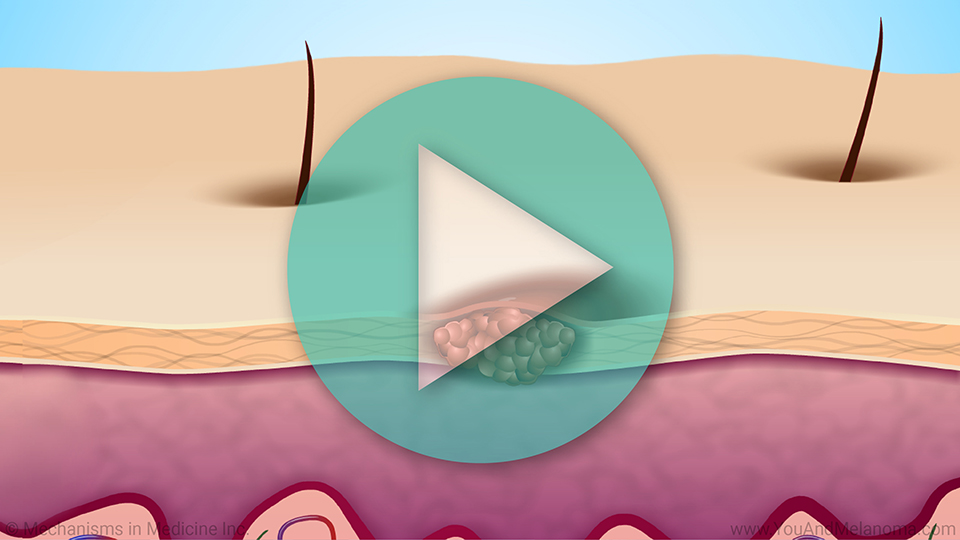
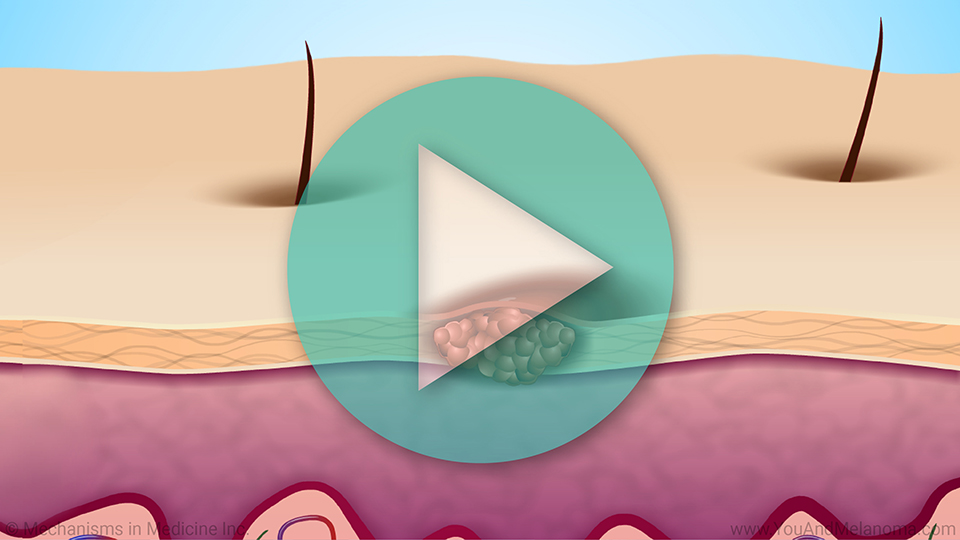
Stage I or II or “local” melanoma is deeper than Stage 0 but still confined to the skin. It starts between the outer skin (epidermis) and inner skin (dermis) and can spread into the inner skin.
In Stage III or “loco-regional” melanoma, cancer cells have spread to nearby skin or to lymph nodes.
In Stage IV or “advanced” melanoma, cancer cells have spread to distant parts of the body.
Research suggests that nine out of 10 melanomas are caused by too much UV exposure.
You can prevent melanoma by using safe sun practices when you are outdoors.
Seek shade. Try to confine outdoor activities to before 10 AM and after 4 PM. The sun’s rays are strongest between 10 AM and 4 PM.
Avoid getting sunburned. Use a broad-spectrum sunscreen with a sun protection factor, or SPF, of at least 30 every day – even in winter, or when it’s cloudy. And, don’t forget to re-apply sunscreen if you are swimming or sweating.
Wear protective clothing if you will be out in the sun for a prolonged period of time. This can include: a long-sleeved shirt, long pants, a wide-brimmed hat, and sunglasses.
Avoid tanning – whether intentionally or unintentionally. And stay away from sun lamps and tanning beds.
And finally, you can be proactive in preventing melanoma by examining your skin carefully once a month.
If you see anything that concerns you, make an appointment right away to have your primary care practitioner or dermatologist examine your skin.
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about melanoma which will help other patients, caregivers and families.










This educational activity has been developed by the Melanoma Research Foundation (MRF), and Mechanisms in Medicine Inc.
This activity is supported by independent educational grants from Bristol-Myers Squibb, Foundation Medicine, Genentech, Iovance Biotherapeutics, Merck, Natera, and Novartis.







This website is part of the Animated Patient™ series developed by Mechanisms in Medicine Inc., to provide highly visual formats of learning for patients to improve their understanding, make informed decisions, and partner with their healthcare professionals for optimal outcomes.

